Key Points:
- 1. Therapeutic alliance
- 2. Therapeutic fit
- 3. Compass for change
In the space of mental health, the importance of the therapeutic alliance is essential. It can be described as the trusting and collaborative relationship between a client and therapist that forms the cornerstone of successful therapy outcomes (Cuncic, 2023). This bond goes beyond professional interaction; it is a dynamic connection that fosters an environment where personal development and change can prosper (Ardito & Rabellino, 2011).
One key aspect of this alliance is the concept of the right therapeutic fit. Just as every individual is unique, so too are their needs and preferences in therapy. The right therapeutic fit is the interplay between a client and therapist where personalities, communication styles, and therapeutic approaches align. Like a tailor-made outfit, the right fit ensures that the therapeutic process is not only effective but also comfortable for the client.
When clients feel a genuine connection with their therapists, it creates a safe space for vulnerability, authenticity, and self-exploration – which serves as the greatest indicator of therapeutic success. A mismatch, conversely, can impede progress and leave clients feeling unheard, unresolved, or misunderstood.
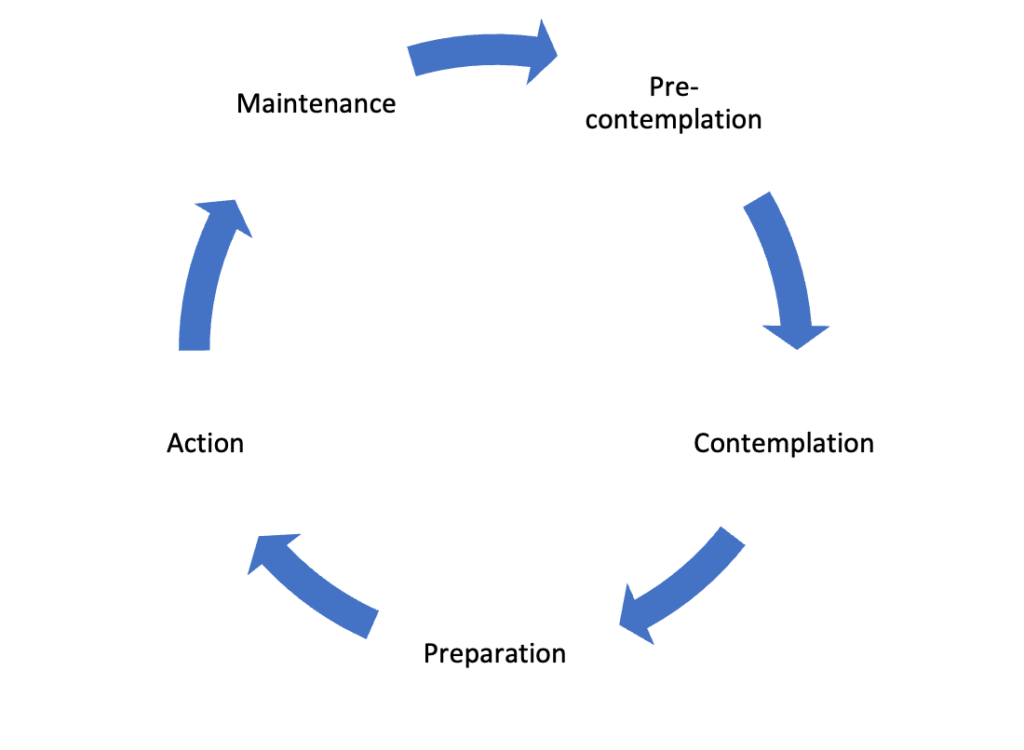
Therapists who prioritize establishing a strong therapeutic alliance demonstrate empathy, trust, respect, active listening, and a genuine commitment to their clients’ well-being. The therapeutic alliance is not established overnight, however as clients navigate the often-challenging journey of self-discovery and growth, the therapeutic alliance becomes the compass guiding them toward healing and resilience. Research shas shown that the quality of therapeutic alliance acts as a dependable predictor of positive therapeutic engagement, motivation and clinical outcome – independent of the psychotherapeutic approach used (Ardito et al., 2011).
In essence, the therapeutic alliance and the right therapeutic fit are not just abstract concepts; they are the heart and soul of effective therapy. By recognizing and nurturing this alliance, clients and therapists co-create a transformative space where change and personal growth become not only possible, but probable.
Tips to make your therapy experience better include giving it a few sessions before deciding if the therapeutic alliance/fit feels right, not being afraid to ask questions about the process, making sure you feel heard, seen, understood and collaborated with, expressing your needs, providing feedback to your therapist, reflecting on your therapy journey, and keeping the lines of communication open about your changing goals and needs.
Natasha Vujovic, M.Psy, R.P (Q) is a Registered Psychotherapist (Qualifying) at CFIR. She works with individuals and couples experiencing a wide range of psychological and relational difficulties including anxiety and stress, depression, mood and grief, relational conflict, trauma, life transitions, personality, body-image, marital and pre-marital, internal conflicts, family dynamics and self-esteem. Natasha is an integrative therapist pulling from psychodynamic/analytic theories and takes a collaborative and honest approach to session.
References:
Ardito, R. B., & Rabellino, D. (2011). Therapeutic alliance and outcome of psychotherapy: historical excursus, measurements, and prospects for research. Frontiers in Psychology, 2, 270. https://doi.org/10.3389/fpsyg.2011.00270
Cuncic, A. (2023, November 30). Why a Therapeutic Alliance Is Important in Therapy. Verywell Mind. https://www.verywellmind.com/the-therapeutic-alliance-2671571